Check out the Language Fundamentals / SLP Communication Foundations Blog!
Recent Posts

Case Mix Limbo – Welcome to New York
New York State recently froze Medicaid rates for...

The Hidden Value of Mobile FEES
Flexible Endoscopic Evaluations of Swallowing...

FEES – A Brief History
Although Flexible Endoscopic Evaluation of...

New CPT Codes Streamline Caregiver Training in Therapy Services
We’ve all been there – medical professionals...
Choose a category…
Skilled Nursing Facility Posts

The Hidden Value of Mobile FEES
Flexible Endoscopic Evaluations of Swallowing (FEES) are an essential component of the diagnosis...

FEES – A Brief History
Although Flexible Endoscopic Evaluation of Swallowing (FEES) dates back to 1988 by Dr Susan...

New CPT Codes Streamline Caregiver Training in Therapy Services
We’ve all been there – medical professionals have spent countless hours on the crucial training...

Case Mix Limbo – Welcome to New York
New York State recently froze Medicaid rates for payments to SNFs until a new case mix...
PDPM Posts

Case Mix Limbo – Welcome to New York
New York State recently froze Medicaid rates for...
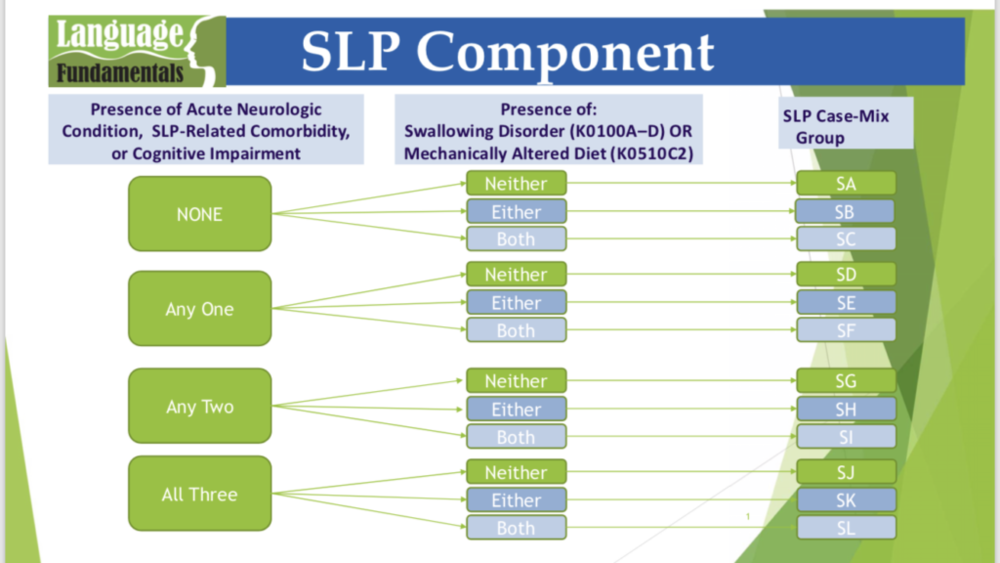
How Does Speech Therapy Impact PDPM? Inside the Numbers
Do you know if speech therapy is truly making a...

Medicare Bootcamp 2023: What’s on the Horizon?
Language Fundamentals leadership recently took...

Speech Therapy’s Skill in Coding Cognitive Impairment Beyond the BIMs
The Patient-Driven Payment Model (PDPM) has...
Early Intervention Posts

Facilitating Language Development at Home
As your child's speech and language skills begin...
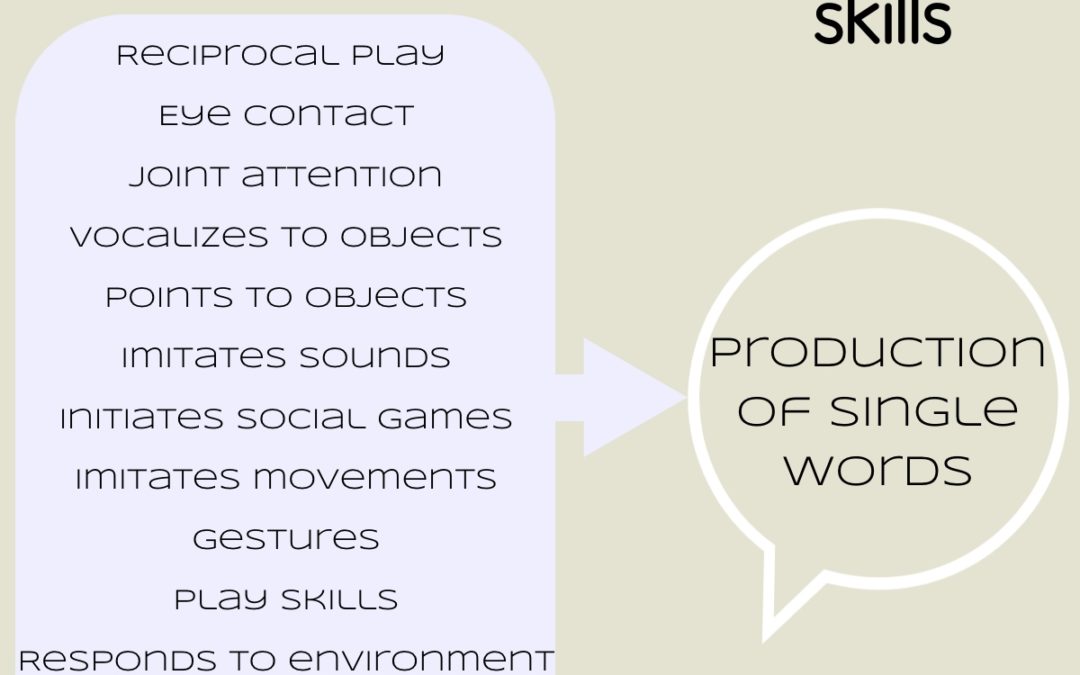
Prelinguistic Skills: What Parents Need to Know
Prelinguistic skills are communication skills...

Turning Gestures into Words: Tips for Toddlers
Do you find yourself looking for tips on how to...

3 Ways to Promote the Early Developing Sound /m/
As babies grow and begin to produce a variety of...
Clinical Resources for Speech-Language Pathologists

The Hidden Value of Mobile FEES
Flexible Endoscopic Evaluations of Swallowing...

FEES – A Brief History
Although Flexible Endoscopic Evaluation of...

New CPT Codes Streamline Caregiver Training in Therapy Services
We’ve all been there – medical professionals...
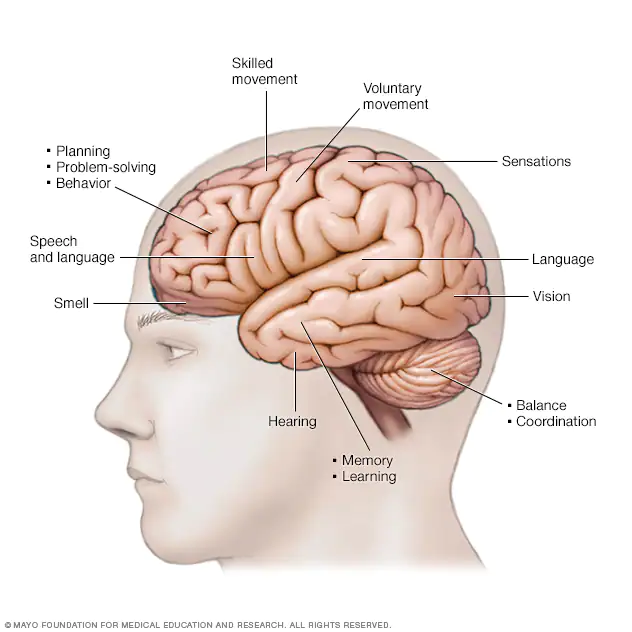
The 3 types of Primary Progressive Aphasia
Primary progressive aphasia (PPA) is a...

